|
Abstract
Purpose: In diabetes, generalised microvascular disease and
coronary artery disease (CAD) are likely to occur in parallel.
We used a sidestream dark field (SDF) handheld imaging device
(Microvascular (blood) image observation
instrument,SDF imaging device)to
determine the relation between the labial microcirculation
parameters and CAD in asymptomatic patients with diabetes.
Methods: SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) was validated for assessment of labial
capillary density and tortuosity. Thereafter, mean labial
capillary density and tortuosity were evaluated and compared in
non-diabetic controls, and in asymptomatic patients with type 1
and type 2 diabetes. In diabetic patients, mean capillary
density and tortuosity were compared according to the presence
of CAD.
Results: Both type 1 and type 2 diabetes were associated with
increased capillary density and tortuosity. In diabetes, mean
capillary density was an independent predictor of elevated
coronary artery calcium (CAC) (p = 0.03) and obstructive CAD on
computed tomography angiography (p = 0.01). Using a cut-off mean
capillary density of 24.9 (per 0.63 mm2) the negative predictive
value was 84% and 89% for elevated CAC and obstructive CAD.
Likewise, capillary tortuosity was an independent predictor of
increased CAC (p = 0.01) and obstructive CAD (p = 0.04).
Conclusion: Assessment of labial microcirculation parameters
using SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) is feasible and conveys the potential to
estimate vascular morbidity in patients with diabetes, at
bedside.
Keywords
Microcirculation, angiogenesis, imaging, diabetes mellitus,
coronary disease
Introduction
Cardiovascular disease, especially coronary artery disease
(CAD), is a predominant cause of morbidity and mortality in
diabetes.1 As a result, recent research has aimed to determine
additional risk factors and markers, to distinguish high risk
diabetic patients.2,3 Likewise, the presence of microvascular
co-morbidities, in the form of nephropathy, retinopathy and
neuropathy, has been previously associated with an increased
risk of CAD as well as its worse prognosis in diabetes.4¨C7
Generalised microvascular disease and CAD may occur in parallel
due to common pathogenic mechanisms initiated by
hyperglycaemia.8 However, microvascular disease has also been
suggested to contribute to CAD directly through angiogenesis of
microvessels in the atherosclerotic plaque.9 As a consequence, a
measure to quantify and qualify microvascular disease in
diabetes may convey the potential to predict vascular morbidity
and CAD more accurately than the traditional risk factors.The
orthogonal polarisation spectral (OPS) and the more novel
sidestream dark field (SDF) handheld imaging device
(Microvascular (blood) image observation
instrument,SDF imaging device)allow direct visualisation of blood in the microcirculation.10,11 Thereby,
the microcirculatory network of arteriolesand capillaries can be
investigated non-invasively. In particular,the technique is
suitable for the study of easily accessible tissues with a
superficial microcirculatory network of the skin and mucous
membranes. Accordingly, OPS and SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) have been applied to
assess the characteristicsof the microcirculation and monitor
its alterations in the nail fold as well as in sublingual and
labial tissue of patients with heart failure, rheumatic diseases
and sepsis.12,13 However, to our knowledge no previous studies
have been performed in patients with diabetes.
In the current study we first sought to validate the assessment
of labial microcirculation parameters, consisting of capillary
density and tortuosity, using the SDF imaging device(sidestream
dark field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument). Secondly,
the labial capillary density and tortuosity were compared in
non-diabetic controls and patients with diabetes. Finally, the
relation between labial capillary density and tortuosity with
CAD was evaluated in the sub-population of patients with
diabetes.
Methods
Study design and population
One hundred and thirty-one consecutive asymptomatic patients
with diabetes were referred to the cardiology outpatient clinic
for cardiovascular screening. The American Diabetes Association
criteria were used to define diabetes and for further
stratification in type 1 or 2.14 Patients were considered as
having type 1 diabetes if laboratory analysis demonstrated
auto-antibodies to islet cells, insulin and glutamic acid
decarboxylase. Otherwise, patients were considered to have type
2 diabetes. Further cardiovascular risk factors were assessed
according to the following criteria: positive family history of
CAD (defined as presence of CAD in first degree family members
younger than 55 (males) or 65 (females) years of age), smoking
(defined as current smoking or smoking in the last two years),
hypertension (defined as a blood pressure >140/90 mmHg or
treatment with antihypertensive medication),
hypercholesterolaemia (defined as a total cholesterol level >
5.0 mmol/L or use of cholesterol lowering medication), degree of
obesity (estimated by body mass index (BMI = kg/m2)), level of
gly caemic control defined by plasma glycated-haemoglobin (mmol/L)
and presence of micro-albuminuria (defined by a urine albumin/creatinine
ratio ¡Ý 3.5 mg/mmol). Second, non-invasive multi-slice computed
tomography (MSCT), including coronary artery calcium (CAC)
scoring and coronary angiography, were performed as part of
clinical work-up. Also, all patients underwent non-invasive
assessment of the labial microcirculation using SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device), to
determine capillary density and tortuosity. The latter was
performed in a study setting, performed according to the
Declaration of Helsinki and approved by the institutional review
committeeof the Leiden University Medical Centre, Leiden. All
patients gave written informed consent.
In addition, as part of the study setting, 50 asymptomatic
healthy individuals constituting the non-diabetic control group
underwent a similar non-invasive assessment of the labial
microcirculation using SDF(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device). The healthy individuals constituting
this control group had no history of diabetes or cardiovascular
disease and were not known to be with related risk factors
(hypertension, hypercholesterolaemia, smoking or micro-albuminuria).
Validation study of the
microcirculation parameters as assessed by SDF
The intra- and interobserver
variability of the labial capillary density and structure was determined in the non-diabetic
control group (N = 50). For this sub-population, SDF imaging of
the four inner lip quadrants was performed by two experienced
observers. SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) was performed twice by each observer, on
two different occasions. Each observer independently performed
processing of their own recordings followed by assessment of the
capillary density and tortuosity.
Assessment of labial
microcirculation
Data acquisition by sidestream
dark field imaging. Imaging of the capillaries was performed
with SDF imaging(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) with a handheld MicroScan
Video Microscope . The SDF device was fitted with
a sterile disposable 5¡Á magnification lens. Video output was
visualised on a monitor and connected to a computer
via a signal converter (Canopus, ADVC110).
Measurements were performed by two trained physicians blinded to
clinical data. All subjects (patients with diabetes and
non-diabetic controls) were instructed to refrain from consuming
caffeine-containing substances 2 h prior to the evaluation.
Subjects were in supine position,in a temperature controlled
room with a temperature of approximately 22¡ãC. The tip of the
SDF probe was placed on the inner lip. To prevent
microcirculatory(SDF imaging device) perfusion disturbance due to application of
pressure on the imaging area, the probe was first placed on the
labial tissue and then retracted to an extent which minimised
contact but enabled visualisation of the capillary bed.
Illumination intensity and depth of focus were modulated to
fine-tune image quality.
Continuous digital image recordings (duration 1 min) were
captured in four quadrants of the inner lip: upper right
quadrant, upper left quadrant, lower right quadrant and lower
left quadrant. Per quadrant, digital image recordings were saved
on a hard drive as DV-AVI files to enable off-line analysis.
Assessment of microcirculation(SDF imaging device). For further assessment of
capillary density and structure, three frozen microcirculatory
imaging areas were selected from the digital image recordings
for each quadrant. Microcirculatory(SDF imaging device) imaging areas wereselected
to meet the following criteria: 1) representative capillary
density and structure for the studied quadrant, 2) longitudinal
axis view with full-length capillaries enabling structural as
well as quantitative assessment of the capillaries, 3) clear,
well-focused view of the capillaries. Each microcirculatory
imaging area visualised by SDF(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) corresponded with a tissue area
of 0.63 mm2 (0.9 mm ¡Á 0.7 mm) (Figure 1).
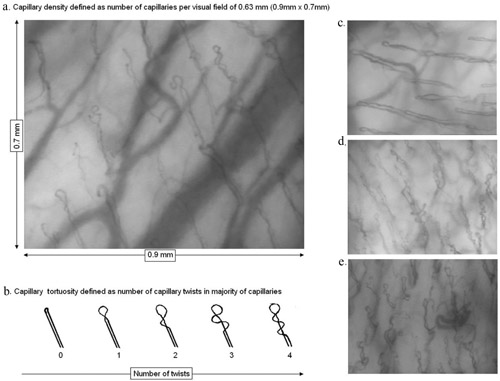
Figure 1. Visualisation of the labial micro-vasculature by
sidestream dark field(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device). Capillaries are identified as loops
emerging from the wider arterioles in the background (a, c¨Ce).
To assess capillary density the number of capillaries was
determined in a visual field of 0.63 mm2 (a). To assess
capillary tortuosity, the number of twists per capillary in the
majority of capillaries was evaluated for each patient. Number
of twists was stratified as 0: no twists (or pinhead
capillaries) to 4: four or more twists (b). A relatively low
capillary density and tortuosity score was observed in
non-diabetic controls (c). In contrast, a higher capillary
density and tortuosity score was observed in patients with
diabetes (d), often accompanied by dilation, branching and
malformation of the capillaries (e).Capillary density. To determine capillary density, the
number of capillaries was counted manually on each selected
microcirculatory(SDF imaging device) imaging area, on the monitor. All vessels
identified as capillaries were included. Partially visible
capillaries were included if the observer was certain that the
vessel was a capillary due to its morphology. Capillary density
was defined as the number of counted capillaries per
microcirculatory(SDF imaging device) image area (capillaries per 0.63 mm2) (Figure
1). Finally, capillary density of the 12 microcirculatory
imaging areas (three microcirculatory(sidestream dark
field (SDF) handheld imaging device,Microvascular
(blood) image observation instrument,SDF imaging device) imaging areas per
quadrant) were averaged to obtain the mean capillary density per
subject.
Capillary tortuosity. To assess the capillary tortuosity
score, the number of twists per capillary in the majority of
capillaries was evaluated, on each selected microcirculatory(SDF imaging device)
imaging area. The number of twists was stratified as 0: no
twists (or pinhead capillaries) to 4: four or more twists
(Figure 1). Subsequently, the overall tortuosity score per
subject was determined by selecting the most frequent tortuosity
score in the 12 studied microcirculatory imaging areas.......etc. |