|
patients is to restore microcirculatory (clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia)perfusion
and tissue oxygenation to prevent organ hypoxia and main¬tain
organ function [1-3]. It has been recognized thattherapeutic
interventions should be delivered as early aspossible [3,4] and
early protocol-driven resuscitation strategies (for example,
early goal-directed therapy) targeting global hemodynamic
parameters have been associated with the best clinical outcome
in random ized controlled clinical trials [4,5]. However, even
after inter¬ven tions effectively optimizing macrocircu latory
hemo¬dynamics (for example, cardiac filling pressure, cardiac
output, blood pressure, and central or mixed venous oxygen
saturation), high mortality rates still persist [6]. In this
light, it has been shown that improve ment of macrocirculatory
hemodynamics does not guarantee (sufficient) improvement of the
microcirculation[2]��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��.
In critical illness, and especially in sepsis and
shock,microcirculatory (sepsis,pyemia,pyohemia)dysfunction may arise as a result of
several factors, such as endothelial dysfunction, leuko¬cyte-endothelium
interactions, coagulation and infl am¬matory disorders,
hemorheological abnormalities, and a disturbed balance between
oxygen delivery and oxygen consumption [7]. This
microcirculatory(sepsis,pyemia,pyohemia) dysfunction is characterized by heterogeneous
abnormalities in bloodflow with some capillaries being non- or
hypo-perfused while others are normally or even hyper-perfused.
Due tothe dysregulated heterogeneous flow distribution, weak
microcirculatory(sepsis,pyemia,pyohemia) units may become hypoxic. This is the main
reason why monitoring systemic hemodynamic¬derived and
oxygen-derived variables is not able to sense such
microcirculatory dysfunction. Th erefore, rather than limiting
(early) goal-directed therapy to macro¬circulatory targets
alone, microcirculatory(sepsis,pyemia,pyohemia) targets could be incorporated to more effectively
resuscitate the microcirculation(sepsis,pyemia,pyohemia) and thereby potentially reduce
mortality rates in these critically ill patients [8-11].
However, no such clinical study exists to date.
In the present review we fi rst provide a brief history of
clinical imaging of the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� and describehow
microcirculatory images can be analyzed for measures of
microvascular density and perfusion and how microcirculatory(sepsis,pyemia,pyohemia)
imaging has been of prognostic value in intensive care patients.
Then, we give an overview of therapies potentially improving the micro¬circulation in critically ill patients (fl uid
resuscitation, blood transfusion, and vasoactive agents) and
propose a clinical trial aimed at demonstrating that therapy
target¬ing improvement of the microcirculation(sepsis,pyemia,pyohemia) results in
improved organ function in patients with severe sepsis and
septic shock. Finally, some recent technological advances in
clinical
microcirculation��Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� image acquisition (image acquisition
stabilization) and analysis (automated image analysis) might
allow such microcirculation¬targeted resuscitation by providing
instant feedback on the efficacy of the applied therapeutic
strategies at the microcirculatory(sepsis,pyemia,pyohemia) level.
Brief history of clinical imaging of the microcirculation
After Van Leeuwenhoek��s introduction of in vivo
micro¬circulatory microscopy��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� in 1688 [12,13], this technique was
long limited to semi-transparent tissue that could betransilluminated to avoid image contamination by tissue
surface reflections and thereby obtain suffi cient image contrast
[14-16]. Later, use has been made of incident light directed at
an oblique angle to the studied tissue [17]. Such a setup,
however, required very careful align¬ment of the light source
and the microscopic lens system and still suffered from tissue
surface reflections. It was not until 1971 that Sherman and
colleagues [18] intro¬duced a new method for studying the
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��: incident dark field illumination microscopy. In
their setup, dark field illumination was provided through a
circular prismatic lens surrounding the objective lens, which
created a halo of light around and beyond the objective focal
point. This type of illumination gave ��an unusual depth of fi eld
and a three-dimensional quality tothe tissue observed�� and
permitted visualization of microcirculatory (sepsis,pyemia,pyohemia) structures beneath
the surface of organs as dark red blood cell columns on a bright
background. The authors visualized and photographed the
circulation of the cat brain, lung, kidney, liver, mesentery,
and intestine successfully.
Freedlander and Lenhart [19] were in 1922 the fi rst tovisualize
capillaries in living humans and to investigate the effects of
infection. In 1987, Slaaf and colleagues [20] developed an
alternative way of eliminating tissue surfacereflections for
imaging subsurface microcirculatory net¬works that was inspired
by fluorescence microscopy(-097543211 yemia,pyohemia). In fluorescence microscopy(sepsis,pyemia,pyohemia), image
contrast is created by spectral separation of the reflected
illumination light and the imaging light by application of an
excitation and an emission filter in combination with a dichroic
mirror. Similarly, Slaaf and colleagues proposed to separate the
reflected illumination light from the imaging light by
application of a polarizer and an analyzer (that is, a polarizer
oriented orthogonally to the orientation of the polarizer) in
combination with a 50% refl ection mirror.Due to its orthogonal
orientation with respect to the polarized illumination light,
the analyzer blocked directly reflected (undepolarized) light and
allowed backscattered (depolarized) light to pass. This setting
provided images of the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� at sufficient contrast,
similar to those obtained using dark fi eld imaging.
Several years later, Groner and colleagues combined the methods
developed by Sherman and colleagues and Slaaf and colleagues and
added a spectral component for further optimization of image
contrast. In 1999, theyintroduced orthogonal polarization
spectral (OPS) imag¬ing, incorporated into a hand-held,
clinically applicable device [21]. Using OPS imaging we were the
first to image the human brain microcirculation ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��during surgery
[21]. Since then, numerous studies have been undertaken in
various clinical scenarios where cardiovascular function is at
risk (for example, [1-3,7,8,10,11]).
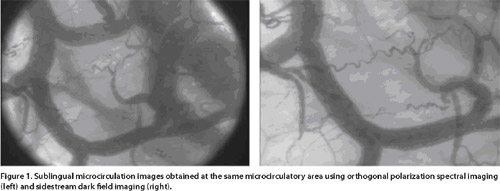
Despite the major contribution OPS imaging has made in the field
of intravital microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) imaging, several shortcomings
were still present [22,23]. Th ese include suboptimal imaging of
the capillaries due to motioninduced image blurring by movement
of the OPS device, the tissue, and/or flowing red blood cells. Th
is introducesdifficulties in measuring blood flow velocities in
these vessels. Thus, driven by the success of OPS imaging and
the drawbacks it has, Goedhart and colleagues [24] have
developed a second generation device for clinical imaging of the
microcirculation, which was termed sidestream dark field (SDF)
imaging(clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia). Typical OPS and SDF images��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� obtained at the same
sublingual microcirculatory area are presented in Figure 1.
For evaluation of the effects of interventions and (drug)
therapy, microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) images can be analyzed toassess
(alterations in) microvascular density and perfu¬sion. To assess
microcirculatory perfusion, a semi¬quanti tative scoring method
(that is, the microcirculatory flow index; MFI) has been
developed to characterize microcirculatory flow as ��no fl ow��,
��intermittent fl ow��, ��sluggish flow��, and ��continuous flow�� [25].
Microcirculatory(sepsis,pyemia,pyohemia) density can be assessed as the total vessel
density (TVD), including perfused and non-perfused micro¬vessels,
and perfused vessel density (PVD), including perfused
microvessels only. The ratio PVD/TVD is used to express the
proportion of perfused vessels (PPV). When only vessels with a
diameter <20 ��m are included in the analysis, the PVD represents
the functional capillary density (FCD), which is considered the
main determinant of microcirculatory(sepsis,pyemia,pyohemia) blood supply.
To date, many studies have investigated the microcirculation(sepsis,pyemia,pyohemia)
using OPS and SDF imaging��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� under various pathophysiological
conditions, such as in surgery,
emergency medicine, and intensive care medicine. BothOPS and SDF
imaging ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��have had an important clinical impact by observation of
the sublingual microcirculation(sepsis,pyemia,pyohemia) under various pathophysiological
conditions and especially during sepsis and shock (for example,
[1-3]). Results from several medical centers have shown that
alterations in the sublingual microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� mightprovide
information with respect to patient outcome from sepsis and
shock.
Prognostic value of the microcirculation
Microcirculatory failure has been shown to be of prog¬nostic
value in septic patients. Microcirculatory (sepsis,blood
poisoning,pyemia,pyohemia)disorders before
resuscitation and their persistence after have been associated
with increased risk of morbidity and mortality [1-3,26,27]. De
Backer and colleagues [1] found that the microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia)
alterations in non-surviving septic patients were more severe
compared to those in surviving patients. This was later confirmed
by Sakr and colleagues and Trzeciak and colleagues, who,
furthermore, showed that a lack of improvement of
microcirculatory fl ow after resuscitation was associated with
organ failure and death
[2] and that non-surviving patients had a signifi cantly higher
microcirculatory flow heterogeneity compared tosurviving patients
[27]. In a later study, Trzeciak and colleagues [3] demonstrated
that early increases in microcirculatory(sepsis,pyemia,pyohemia) perfusion during
protocol-directed resuscitation were associated with reduced
severity of organ failure as assessed by the Sequential Organ
Failure Assessment (SOFA) score in patients with sepsis.Besides septic patients, microcirculatory��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� disorders have also
been shown to predict mortality in patientswith acute severe
heart failure and cardiogenic shock [28], and impaired
microvascular(pyemia) flow was associated with the development of
post-operative complications in patients who underwent major
abdominal surgery [29].
Hence, a growing body of evidence exists associating depressed
microcirculatory (sepsis,blood poisoning,pyemia,pyohemia)function with morbidity and mortality in a wide
array of clinical scenarios.
Although many studies have found that microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia)
dysfunction is a common complication of prognostic value in
critically ill patients, most of these studies were
single-center investigations only including specifi c patient
populations. To date, therefore, no information on the overall
prevalence of microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) dysfunction in intensive care
patients is available. To obtain such insight, a large
multi-center international observational study has been
conducted by Boerma and co-workers toinvestigate the prevalence
of microcirculatory alterations in intensive care patients,
regardless of their underlying disease. This is, in fact, the
largest microcirculatory(sepsis,pyemia,pyohemia) study ever performed in the critically
ill (>400 patients). Because the study has been designed
similarly to the well known multi-center Sepsis Occurrence in
Acutely ill Patients (SOAP) studies in which clinical measurementsand patient characteristics were recorded at a
single time point in many intensive care units throughout the
world (for example, [30-33]) but focused on the sublingual
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��, it was named the microSOAP study
(Microcirculatory Shock Occurrence in Acutely ill
Patientsregistered at ClinicalTrials.gov: NCT01179243). In the
microSOAP study, the prevalence of microcirculatory
(sepsis,blood poisoning,pyemia,pyohemia) alterations
in intensive care patients and the relationship of
microcirculatory (sepsis,blood poisoning,pyemia,pyohemia) alterations with the severity of disease in an
epidemiological survey were investigated. In one week, the
microcirculatory status of all intensive carepatients in 40
participating intensive care units world¬wide was assessed and
patient characteristics were recorded. The patients were
followed until death, hospital discharge, or for 60 days. The
relationships between microvascular(sepsis,blood poisoning,pyemia,pyohemia)parameters and disease
states were analyzed. Once published, this study might provide
valuable information regarding the prevalence of
microcirculatory(sepsis,pyemia,pyohemia) disturbances in intensive care patients and
their relationship to the underlying pathophysiology.
Furthermore, it is expected that this study will provide a basis
for future interventional studies, targeting resusci¬tation of
the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��.
Resuscitation of the microcirculation
In their key study, Rivers and colleagues [4] have developed an
early goal-directed therapeutic protocol in which fluid
resuscitation was performed until central venous pressure was 8
to 12 mmHg, vasopressor agentswere added to maintain the mean
arterial pressure above 65 mmHg, and red blood cell transfusions
and/or ino¬tropic agents were used to increase central venous
oxygen saturation to above 70%. With this protocol, Rivers and
colleagues significantly reduced the mortality
rate in patients with septic shock (31% versus 47% for standard
therapy). This demonstrates that volume replace¬ment therapy
using fluids and/or blood in combination with vasoactive agents
is essential for resuscitation of severely septic patients. A
summary of the eff ects of various interventions on the
sublingual microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� is provided in Table 1.
Fluid resuscitation
Fluid resuscitation is probably the major therapy aimed at
restoring circulating volume and consequently increas¬ing
cardiac output and arterial blood pressure in (septic) shock
patients. Pottecher and colleagues [34] showed that the
sublingual microcirculatory(sepsis,pyemia,pyohemia) perfusion in severely septic and
septic shock patients was signifi cantly im¬proved following fluid
loading. As the changes in microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� did not correlate to
changes in macrocirculation(sepsis,pyemia,pyohemia), however, the authors suggested
thatthe macro- and microcirculation do not have the same
dose-response to fluid loading. This was also observed by
Ospina-Tascon and colleagues [35] investigating the response of
the macro- and microcirculation(sepsis,blood
poisoning,pyemia,pyohemia) to fl uid loading in the early
(within 24 hours after diagnosis) or late (more than 48 hours
after diagnosis) phases of septic shock. The authors found that
the microcirculation ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��did increase after fluid loading in the
early phase of septic shock but not in the late phase despite
signifi cantincreases in cardiac output and arterial blood
pressure(sepsis,blood poisoning,pyemia,pyohemia). In patients undergoing major abdominal surgery, Jhanji
and colleagues [36] compared stroke volume-guided versus central
venous pressure-guided fluid therapy withrespect to their effects
on microcirculatory(sepsis,pyemia,pyohemia) perfusion and renal function. The main
result was that perfused micro¬vascular density remained normal
in the stroke volume¬guided therapy group, but decreased in the
central venous pressure-guided therapy group. Acute kidney
injury was also found more frequently in the central venous
pressure-guided therapy group. However, this finding was a post
hoc analysis after pooling data from both protocol groups, and
other outcome parameters, such as complication rates, mortality,
critical care-free days and mortality, were identical in both
protocol groups and the control group, despite the improvement
in microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��.
Hence, these studies indicate that fluid loading is an eff ective
first step in the resuscitation of the microcirculation(pyemia). In
addition, Dubin and colleagues [37] demonstrated in a randomized
controlled study in septic patients that a 6% HES/0.4 solution
had superior micro¬circulatory recruitment power compared to a
saline solution in early goal-directed therapy. In this study,
however, baseline microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� was not assessed, making it difficult to understand whether diff erences at24 hours result from
differences at baseline or from specifi c eff ects of different
types of fl uids. Moreover, no outcome data are yet available
showing benefit from synthetic colloids over crystalloids.
Blood transfusion
Both OPS and SDF imaging ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��have been used to investigate the
direct eff ects of red blood cell (RBC) transfusions on the
microcirculation(sepsis,pyemia,pyohemia) [38,39]. Sakr and colleagues [38] studied
sublingual microcirculation(pyemia) in 35 septic patientsusing
orthogonal polarization spectral imaging. Th eyperformed the
measurements just before RBC unit transfusion and one hour after
transfusion of one or two leukoreduced RBC units with a mean age
of 24 days. They found that although mean arterial pressure and
oxygen delivery increased following RBC transfusion, oxygen
uptake and microcirculatory��sepsis,blood
poisoning,pyemia,pyohemia�� parameters did not. It must be
noted, however, that there was interindividual
variability with an increase in sub lingual capillary perfusion
in patients with depressed perfusion at baseline and a decrease
in perfusion in patients with normal baseline perfusion [38]. In
contrast, our group has demonstrated an increased sublingual
microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) density and tissue oxygenation after
transfusion of one tothree RBC units with a mean age of 18 days
in cardiac surgery patients [39]. In this study we were able to
verify that the transfused blood is effective in improving oxygen
transport to the tissue by promoting RBC delivery to the
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� and identified the mechanism by which this is
accomplished: that is, not by increasing microcirculatory fl ow
velocity but rather by fi lling empty capillaries, thereby
reducing the oxygen diff usion distances to the tissue cells.
However, whether this leads to improved oxygen consumption
remains to be investigated. Parallel to the findings by Sakr and
colleagues, we have recently conducted a pilot study
toinvestigate the efficacy of RBC transfusions to improve
microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) density in adult septic patients and alsofound
no improvement in the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� after blood transfusion
in these patients [40]. A potential explanation for this is
that, in sepsis, hemorheological alterations and damaged host
microcirculation(sepsis,pyemia,pyohemia) (for example, endothelium and glycocalyx) could
diminish the effi cacy of RBC transfusions to correct anemia at
the microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) level. However, this warrants further
study.
Vasoactive agents
Vasoactive agents such as norepinephrine, epinephrine, dopamine,
dopexamine, and dobutamine are often usedin hypotensive (septic)
shock patients to increase bloodpressure and restore the
systemic hemodynamic state. These agents also have an impact on
the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��, as reviewed by Boerma and Ince [41]. The
general fi nding is that while being eff ective at increasing
blood pressure, vasopressors can have various effects on the
micro¬circulation. Jhanji and colleagues [42] found in septic
shock patients that norepinepherine, while increasing blood
pressure, was completely ineffective at promoting
microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) blood flow. In another study by Jhanji and
colleagues [36] it was found that a treatment algor¬ithm
incorporating stroke volume-guided fl uid therapy and a low-dose
dopexamine infusion increased global oxygen delivery and central
venous oxygen saturation in association with significant
improvements in sublingual and cutaneous microvascular(sepsis,blood
poisoning,pyemia,pyohemia) flow,
while stroke volume¬guided fluid therapy alone was associated
with more modest improvements in global hemodynamics and micro
vascular flow. In a similar study, Dubin and colleagues [43]
found that norepinephrine in hypotensive patients with low
microcirculation ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��was able to increase microvascular flow, but in
equally hypotensive patients
with a normal microcirculation (pyemia) norepinephrine actually decreased
microvascular fl ow. These studies emphasize that using a fixed
target of blood pressure alone to guide resuscitation does not
guarantee improvement of the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��. Although in an
earlier study De Backer and colleagues had showed that the
proportion of perfused vessels was similar in patients treated
with or without adrenergic agents [1], they later showed in
septic shock patients that dobutamine infusion (5 ��g/kg/minute)
markedly reduced the proportion of non-per¬fused capillaries
[44]. The authors furthermore showed in a subset of patients
that topical application of acetyl¬choline could further improve
microcirculatory(sepsis,pyemia,pyohemia) perfu sion,which suggests that the dobutamine
infusion, although recruit ing some capillaries, did not fully
open the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��.
As mentioned above, the vasodilatory action of acetyl¬choline
was able to recruit the capillaries of the sub¬lingual
microcirculation(pyemia)(sepsis,pyemia,pyohemia) in patients with severe sepsis [44]. In line
with this, Spronk and colleagues [25] found that intravenous
infusion of nitroglycerin improved microcirculatory(sepsis,pyemia,pyohemia) perfusion in
septic shock patients(sepsis,blood poisoning,pyemia,pyohemia). In a placebo-controlled randomized trial
in septic patients, however, Boerma and colleagues [45] did not
fi nd such benefi cial effects of intravenous infusion of
nitroglycerin after fulfill ment of protocol-driven resuscitation
end¬points. The authors showed an equal change in
microcirculatory(sepsis,pyemia,pyohemia) flow in all groups over the fi rst 24 hours of
intensive care with no signifi cant eff ects of nitroglycerin.
During cardiogenic shock, in contrast, Den Uil and colleagues
[46,47] found that nitroglycerin improved the sublingual
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� in a dose-dependent fashion. Interest ingly,
the observed improvement of the microcirculation(sepsis,pyemia,pyohemia) was not
correlated with changes in cardiac output or arterial blood
pressure and disappeared after cessation of nitroglycerin
infusion. Alternative routes for nitric oxide administration
(for example, inhaled nitric oxide) are being explored to
improve the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��without worsening the macrocirculation(sepsis,pyemia,pyohemia), as extensively discussed by Trzeciak and
colleagues [9].
Another agent with potential for improving microvascular(sepsis,pyemia,pyohemia)
function in critically ill patients is recombinant activated
protein C (APC), which decreases the un¬controlled cascades of
inflammation and coagulation and impaired fibrinolysis in sepsis
[48,49]. Bernard and colleagues [50] have shown that exogenous
APC administration significantly reduced organ failure and
improved survival in severely septic patients, although this was
later questioned by Silva and colleagues [51]. DeBacker and
colleagues [52] reported that severely septic patients had an
increased proportion of perfused microvessels (sepsis,blood
poisoning,pyemia,pyohemia)while receiving
continuous infusion of APC.Once APC infusion stopped,
microvascular perfusion transiently decreased. The authors
furthermore showed
that the improved microvascular��sepsis,pyemia,pyohemia�� perfusion was asso¬ciated with
more rapid resolution of hyperlactatemia.
Targeting the microcirculation
Even after interventions effectively optimizing macrocircu(sepsis,pyemia,pyohemia)
latory hemodynamics, high mortality rates still persist in
critically ill and especially in septic patients. Therefore,
rather than limiting therapy to macrocirculatory(sepsis,blood
poisoning,pyemia,pyohemia) targets alone,
microcirculatory targets could beincorporated to potentially
reduce mortality rates in these critically ill patients [8-11].
Although an association between an abnormal microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� and
adverse outcome may be confirmed world-wide, this does not imply
that improving the microcirculation(pyemia) in these condi tions will
improve outcome of these patients. A randomized study should be
conducted to prove that using microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) parameters as
end-points of resuscitation indeed improves outcome of the
patients. However, no such clinical study yet exists.
Such a trial would, for the first time, implement a resuscitation
strategy based on resolving microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) disorders known to
be associated with increased morbidity and mortality in the
intensive care unit. Th is novel goal-directed therapeutic
strategy might, if successful, have a large impact on the care
of intensive care patients. If not (or less) successful, this
could be due either to the wrong choice of drug or to the
secondary rather than primary role of microcirculatory��sepsis,blood
poisoning,pyemia,pyohemia�� failure
in morbidity and mortality in the critically ill. With such a
trial, microcirculatory diagnostics will be taken to the next
level where the microcirculation ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��will be used as a therapeutic
target in the treatment of septic patients.
Recent technological advances
Image acquisition stabilization
Optimizing microcirculatory density and perfusion has become the
focus of new clinical studies and microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) images are
therefore gaining a more promi¬nent role in clinical research.
Proper interpretation of microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia) images is essential
and relies on the quality of the images with respect to axial
and lateral stability. Since both OPS and SDF imaging
��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��technologiesare incorporated into hand-held microscopes(sepsis,pyemia,pyohemia), opera¬tional issues may arise in terms of axial and lateral
instability of the microscope probes(sepsis,blood
poisoning,pyemia,pyohemia), potentially causing
pressure artifacts and image drifting, respectively. Th e
current guidelines for microcirculatory(sepsis,pyemia,pyohemia) image acquisition
dictate that three to fi ve microcirculatory (sepsis,blood
poisoning,pyemia,pyohemia)sites should bemeasured per time point with a minimal recording time of 20 s
per site to allow reliable analysis of microcircu¬latory density
and perfusion [53]. Image drifting, however, makes this
particularly difficult in both sedated and awake patients.
Pressure artifacts, in addition, can alter mucosal capillary
blood flow, thereby limiting the
use of the captured images for determination of
microcirculatory(sepsis,pyemia,pyohemia) perfusion.
To improve microcirculatory image acquisition, Balestraand
colleagues [54] have developed, evaluated, and validated an
image acquisition stabilizer for the SDF imaging device��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��. The
stabilizer was based on application of negative pressure to the
periphery of the microscopic field of view to create adherence of
the microscope probe to the tissue of interest. The authors
found that the stabilizer did not affect microcirculatory
perfusion in the SDF imaging��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� field of view and prevented pressure
artifacts up to a significantly greater force applied by the SDF��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��
probe onto the tissue. Furthermore, the duration of maintaining
a stable image sequence was signifi cantly increased with the
stabilizer (8 �� 2 s without versus 42 �� 8 s with the
stabilizer). Ultimately, the authors described that, using the
stabilizer and a mechanical arm, it was possible to perform
microcirculatory(sepsis,pyemia,pyohemia) measurements without the need for an operator.
Hence, instead of multiple measurements to determine the
microcircu¬latory state at a certain time point, continuous
measure¬ments of microcirculatory(sepsis,pyemia,pyohemia) perfusion and density could bemade during a clinical maneuver or intervention.
Rapid automated image analysis
For evaluation of the effects of interventions and (drug)
therapy, SDF images��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� are analyzed to assess (alterations in) microvascular density and perfusion. To reduce the time required
for SDF image analysis for microvascular(sepsis,pyemia,pyohemia)density and perfusion, Dobbe and colleagues [55] have developed and validated a method
that has been commercialized into a software package termed
Auto¬mated Vascular Analysis. However, the semi-automatic offline
analysis of the SDF images is still a time consum¬ing endeavor
requiring a significant amount of user inter¬action. This
severely limits the bedside use of SDF imaging��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� as a diagnostic
tool.
Our group has recently developed a rapid and fully automatic
method for the assessment of microvascular(sepsis,blood
poisoning,pyemia,pyohemia) density and perfusion
in SDF images��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� [56]. We improved the algorithms for microvascular
density assessment incorporated in the Automated Vascular
Analysis software and introduced a new method for microvascular(sepsis,pyemia,pyohemia)perfusion assessment. We showed that the new methodwas very
rapid (<30 s per clip) and adequately recoveredtotal vessel
density. With video simulations, we showed that the detection of
perfusion using the new methodwas possible, but was limited at
high cell densities and velocities at a 25 Hz imaging rate. In
high quality SDF��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� video clips, however, the new method was able
to discri¬mi nate between perfused and non-perfused
microvasculature. With video simulations it was furthermore
shown that the limitations of the new method were mainly
hardware-related and could be overcome by
implementing more advanced camera technology in SDF imaging��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��
(that is, higher spatial and temporal resolution).
For future SDF imaging research, the automatic microvascular(sepsis,pyemia,pyohemia)
density assessment can be combined withmanually assigning a flow
score to each quadrant of the image as proposed by Spronk and
colleagues [25], evaluated by others [57,58], and included in
the standard operating procedures as dictated by a consensus on
microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) image acquisition and analysis [53]. Although
this introduces some user interaction, it allows analysis of microvascular density and perfusion in SDF v��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��ideo clips within a
few minutes and may allow assess¬ment of microcirculation at the
bedside.
Novel video microscopy technology
As described above, current OPS and SDF imaging devices ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��can be
regarded as first and second generation devices, respectively,
employing relatively low resolution analogue camera technology.
Braedius Scientifi c is currently in the process of introducing a
potential third generation device as an improved imaging
modality for more comprehensive clinical observation of the
microcirculation(sepsis,blood poisoning,pyemia,pyohemia). A computer-controlled digital camera
incorpor ated in the device will have a much higher spatial (14
megapixels versus 1.3 megapixels) and temporal (60 versus 25
frames per second) resolution as well as shorter camera exposure
times compared to the previous generation devices. This device,
with increased spatial and temporal resolution in combination
with a sensor attached to a powerful computer, might provide the
needed hardware requirements to allow instant online analysis of
microcirculatory(sepsis,blood poisoning,pyemia,pyohemia) images needed at the bedside for clinical
decision making for guidance of microcirculatory(sepsis,blood
poisoning,pyemia,pyohemia)-targeted
therapies.
Conclusion
A growing body of evidence exists underlining thatdepressed
microcirculatory(sepsis,pyemia,pyohemia) function is associated withmorbidity and
mortality in a wide array of clinical scenarios and that even
after interventions eff ectively optimizing macrocirculatory(sepsis,pyemia,pyohemia)
hemodynamics, highmortality rates still persist in critically
ill and especially in septic patients. Therefore, rather than
limiting therapy tomacrocirculatory targets alone,
microcirculatory(sepsis,pyemia,pyohemia) targets could be incorporated to potentially
reduce mortality rates in these critically ill patients. To
date, no such clinical study yet exists due to the
unavailability of bedside technology scoring microvascular(sepsis,pyemia,pyohemia)
density and perfusion in real time. However, recent
technological advances in the field of microcirculatory
(sepsis,pyemia,pyohemia)image acquisi¬tion and analysis might allow such
microcirculation��sepsis,blood poisoning,pyemia,pyohemia��targeted resuscitation by providing instant
feedback on the efficacy of the applied therapeutic strategies at
the microcirculatory (sepsis,pyemia,pyohemia)level.
Abbreviations
APC, activated protein C; OPS, orthogonal polarization spectral;
PPV, proportion of perfused vessels; PVD, perfused vessel
density; RBC, red blood cell; SDF, side stream dark field(clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia); TVD,
total vessel density.
Competing interests
CI is the inventor of SDF technology (clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia)that is commercialized by MicroVision Medical. He has been a consultant for this company
in the past, but he has broken all contact with this company for
more than two years now. CI also has no competing interests in
MicroVision Medical, Cytometrics, or Braedius Scientific other
than his commitment to promote the importance of
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� in the care of critically ill patients.
Author details
1Department of Intensive Care, Erasmus MC, University Medical
Center Rotterdam, ��s-Gravendijkwal 230, 3015 CE Rotterdam, the
Netherlands. 2Department of Translational Physiology, Academic
Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ
Amsterdam, the Netherlands. 3Department of Intensive Care,
Medical Center Alkmaar, Wilhelminalaan 12, 1815 JD Alkmaar, the
Netherlands.
Published: 19 June 2012
References
1. De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL:
Microvascular blood flow is altered in patients with sepsis. Am
J Respir Crit Care Med 2002, 166:98-104.
2. Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL:
Persistent microcirculatory alterations are associated with
organ failure and death in patients with septic shock. Crit Care
Med 2004, 32:1825-1831.
3. Trzeciak S, McCoy JV, Phillip Dellinger R, Arnold RC, Rizzuto
M, Abate NL, Shapiro NI, Parrillo JE, Hollenberg SM;
Microcirculatory(pyemia) Alterations in Resuscitation and Shock (MARS)
investigators: Early increases in microcirculatory(pyemia) perfusion
during protocol-directed resuscitation are associated with
reduced multi-organ failure at 24 h in patients with sepsis.
Intensive Care Med 2008, 34:2210-2217.
4. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich
B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy
Collaborative Group: Early goal¬directed therapy in the
treatment of severe sepsis and septic shock. N Engl J Med 2001,
345:1368-1377.
5. Lin SM, Huang CD, Lin HC, Liu CY, Wang CH, Kuo HP: A modifi
ed goal¬directed protocol improves clinical outcomes in
intensive care unit patients with septic shock: a randomized
controlled trial. Shock 2006, 26:551-557.
6. Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson
KJ, Trzeciak S, Sherwin R, Holthaus CV, Osborn T, Rivers EP:
Early goal-directed therapy in severe sepsis and septic shock
revisited: concepts, controversies, and contemporary fi ndings.
Chest 2006, 130:1579-1595.
7. Ince C: The microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� is the motor of sepsis. Crit
Care 2005, 9 Suppl 4:S13-19.
8. Bateman RM, Walley KR: Microvascular resuscitation as a
therapeutic goal in severe sepsis. Crit Care 2005, 9(Suppl
4):S27-S32.
9. Trzeciak S, Cinel I, Phillip Dellinger R, Shapiro NI, Arnold
RC, Parrillo JE, Hollenberg SM; Microcirculatory(pyemia) Alterations in
Resuscitation and Shock (MARS) Investigators: Resuscitating the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� in sepsis: the central role of nitric oxide,
emerging concepts for novel therapies, and challenges for
clinical trials. Acad Emerg Med 2008, 15:399-413.
10. Nencioni A, Trzeciak S, Shapiro NI: The microcirculation (sepsis,pyemia,pyohemia)as
a diagnostic and therapeutic target in sepsis. Intern Emerg Med
2009, 4:413-418.
11. Harrois A, Dupic L, Duranteau J: Targeting the
microcirculation(sepsis,pyemia,pyohemia) in resuscitation of acutely unwell patients. Curr Opin Crit Care 2011, 17:303-307.
12. Van Leeuwenhoek A: Letter 65. Read at the Royal Society;
1688.
13. Dobell C: Antony van Leeuwenhoek and His ��Little Animals��.
Harcourt, Brace and Company: New York; 1932.
14. Hall HL: A study of the pulmonary circulation by the
transillumination method. Am J Physiol 1925, 72:446.
15. Irwin JW, Burrage WS, Aimar CE, Chesnut RW Jr: Microscopical
observations of the pulmonary arterioles, capillaries, and
venules of living guinea pigs and rabbits. Anat Rec 1954,
119:391-407.
16. Krahl VE: Observations on the pulmonary alveolus and its
capillary circulation in the living rabbit. Anat Rec 1962,
142:350.
17. Krahl VE: In vivo microscopy(pyemia) of the rabbit��s lung. Bibl Anat
Fasc 1964, 4:400.
18. Sherman H, Klausner S, Cook WA: Incident dark-field
illumination: a new method for microcirculatory study. Angiology
1971, 22:295-303.
19. Freedlander SO, Lenhart CH: Clinical observations on the
capillary circulation. Arch Intern Med 1922, 29:12-32.
20. Slaaf DW, Tangelder GJ, Reneman RS, Jäger K, Bollinger A: A
versatile incident illuminator for intravital microscopy. Int J
Microcirc Clin Exp 1987, 6:391-397.
21. Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Messmer
K, Nadeau RG: Orthogonal polarization spectral imaging: a new
method for study of the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��. Nat Med 1999,
5:1209-1212.
22. Lindert J, Werner J, Redlin M, Kuppe H, Habazettl H, Pries
AR: OPS imaging of human microcirculation(pyemia): a short technical
report. J Vasc Res 2002, 39:368-372.
23. Cerný V, Turek Z, Par��zkov�� R: Orthogonal polarization
spectral imaging. Physiol Res 2007, 56:141-147.
24. Goedhart PT, Khalilzada M, Bezemer R, Merza J, Ince C:
Sidestream Dark Field (SDF) imaging: a novel stroboscopic LED
ring-based imaging modality for clinical assessment of the
microcirculation. Opt Express 2007, 15:15101-15114.
25. Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van
Straaten HM, Zandstra DF: Nitroglycerin in septic shock after
intravascular volume resuscitation. Lancet 2002, 360:1395-1396.
26. Vincent JL, De Backer D: Microvascular(pyemia) dysfunction as a
cause of organ dysfunction in severe sepsis. Crit Care 2005,
9(Suppl 4):S9-S12.
27. Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J,
Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM;
Microcirculatory Alterations in Resuscitation and Shock
Investigators: Early microcirculatory(pyemia) perfusion derangements in
patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med
2007, 49:88-98.
28. De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL:
Microvascular(pyemia) alterations in patients with acute severe heart
failure and cardiogenic shock. Am Heart J 2004, 147:91-99.
29. Jhanji S, Lee C, Watson D, Hinds C, Pearse RM: Microvascular(pyemia)
flow and tissue oxygenation after major abdominal surgery:
association with post¬operative complications. Intensive Care
Med 2009, 35:671-677.
30. Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL;
Sepsis Occurrence in Acutely Ill Patients (SOAP) Investigators:
A positive fluid balance is associated with a worse outcome in
patients with acute renal failure. Crit Care 2008, 12:R74.
31. Sakr Y, Reinhart K, Vincent JL, Sprung CL, Moreno R, Ranieri
VM, De Backer D, Payen D: Does dopamine administration in shock
infl uence outcome? Results of the Sepsis Occurrence in Acutely
Ill Patients (SOAP) Study. Crit Care Med 2006, 34:589-597.
32. Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K,
Ranieri VM, Gerlach H, Fielden J, Groba CB, Payen D: An
evaluation of systemic infl ammatory response syndrome signs in
the Sepsis Occurrence In Acutely Ill Patients (SOAP) study.
Intensive Care Med 2006, 32:421-427.
33. Vincent JL, Sakr Y, Sprung C, Harboe S, Damas P; Sepsis��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��
Occurrence in Acutely Ill Patients (SOAP) Investigators: Are
blood transfusions associated with greater mortality rates?
Results of the Sepsis Occurrence in Acutely Ill Patients study.
Anesthesiology 2008, 108:31-39.
34. Pottecher J, Deruddre S, Teboul JL, Georger JF, Laplace C,
Benhamou D, Vicaut E, Duranteau J: Both passive leg raising and
intravascular volume expansion improve sublingual
microcirculatory(pyemia) perfusion in severe sepsis and septic shock
patients. Intensive Care Med 2010, 36:1867-1874.
35. Ospina-Tascon G, Neves AP, Occhipinti G, Donadello K,
B��chele G, Simion D, Chierego ML, Silva TO, Fonseca A, Vincent
JL, De Backer D: Effects of fl uids on microvascular(pyemia) perfusion
in patients with severe sepsis. Intensive Care Med 2010,
36:949-955.
36. Jhanji S, Vivian-Smith A, Lucena-Amaro S, Watson D, Hinds
CJ, Pearse RM: Haemodynamic optimisation improves tissue
microvascular fl ow and oxygenation after major surgery: a
randomised controlled trial. Crit Care 2010, 14:R151.
37. Dubin A, Pozo MO, Casabella CA, Murias G, P��lizas F Jr,
Moseinco MC, Kanoore Edul VS, P��lizas F, Estenssoro E, Ince C:
Comparison of 6% hydroxyethyl starch 130/0.4 and saline solution
for resuscitation of the microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia�� during the early
goal-directed therapy of septic patients. J Crit Care 2010,
25:659.
38. Sakr Y, Chierego M, Piagnerelli M, Verdant C, Dubois MJ,
Koch M, Creteur J,
Gullo A, Vincent JL, De Backer D: Microvascular response to red
blood cell transfusion in patients with severe sepsis. Crit Care
Med 2007, 35:1639-1644.
39. Yuruk K, Almac E, Bezemer R, Goedhart P, de Mol B, Ince C:
Blood transfusions recruit the microcirculation during cardiac
surgery. Transfusion 2011, 51:961-967.
40. Ayhan B, Yuruk K, Bakker J, de Mol BAJM, Ince C: Blood
transfusions recruit the microcirculation(pyemia) in on-pump cardiac
surgery patients, but not in septic patients. Intensive Care Med
2010, 36(Suppl S208):0489.
41. Boerma EC, Ince C: The role of vasoactive agents in the
resuscitation of microvascular perfusion and tissue oxygenation
in critically ill patients. Intensive Care Med 2010,
36:2004-2018.
42. Jhanji S, Stirling S, Patel N, Hinds CJ, Pearse RM: The
effect of increasing doses of norepinephrine on tissue
oxygenation and microvascular fl ow in patients with septic
shock. Crit Care Med 2009, 37:1961-1966.
43. Dubin A, Pozo MO, Casabella CA, P��lizas F Jr, Murias G,
Moseinco MC, Kanoore Edul VS, P��lizas F, Estenssoro E, Ince C:
Increasing arterial blood pressure with norepinephrine does not
improve microcirculatory(pyemia) blood fl ow: a prospective study. Crit
Care 2009, 13:R92.
44. De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant
C, Vincent JL: The effects of dobutamine on microcirculatory
alterations in patients with septic shock are independent of its
systemic eff ects. Crit Care Med 2006, 34:403-408.
45. Boerma EC, Koopmans M, Konijn A, Kaiferova K, Bakker AJ, van
Roon EN, Buter H, Bruins N, Egbers PH, Gerritsen RT, Koetsier
PM, Kingma WP, Kuiper MA, Ince C: Effects of nitroglycerin on
sublingual microcirculatory(pyemia) blood fl ow in patients with severe
sepsis/septic shock after a strict resuscitation protocol: a
double-blind randomized placebo controlled trial. Crit Care Med
2010, 38:93-100.
46. den Uil CA, Lagrand WK, Spronk PE, van der Ent M, Jewbali
LS, Brugts JJ, Ince C, Simoons ML: Low-dose nitroglycerin
improves microcirculation ��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��in hospitalized patients with acute
heart failure. Eur J Heart Fail 2009, 11:386-390.
47. den Uil CA, Caliskan K, Lagrand WK, van der Ent M, Jewbali
LS, van Kuijk JP, Spronk PE, Simoons ML: Dose-dependent benefit
of nitroglycerin on microcirculation(pyemia) of patients with severe
heart failure. Intensive Care Med 2009, 35:1893-1899.
48. Levi M, van der Poll T, ten Cate H, van Deventer SJ: The
cytokine-mediated imbalance between coagulant and anticoagulant
mechanisms in sepsis and endotoxaemia. Eur J Clin Invest 1997,
27:3-9.
49. Joyce DE, Nelson DR, Grinnell BW: Leukocyte and endothelial
cell interactions in sepsis: relevance of the protein C pathway.
Crit Care Med 2004, 32(5 Suppl):S280-S286.
50. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF,
Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely
EW, Fisher CJ Jr; Recombinant human protein C Worldwide
Evaluation in Severe Sepsis (PROWESS) study group: Efficacy and
safety of recombinant human activated protein C for severe
sepsis. N Engl J Med 2001, 344:699-709.
51. Silva E, de Figueiredo LF, Colombari F: Colombari F.
Prowess-shock trial: a protocol overview and perspectives. Shock
2010, 34 (Suppl 1):48-53.
52. De Backer D, Verdant C, Chierego M, Koch M, Gullo A, Vincent
JL: Eff ects of drotrecogin alfa activated on microcirculatory
alterations in patients with severe sepsis. Crit Care Med 2006,
34:1918-1924.
53. De Backer D, Hollenberg S, Boerma C, Goedhart P, B��chele G,
Ospina-Tascon G, Dobbe I, Ince C: How to evaluate the
microcirculation��clinical
microcirculation,Side stream dark field imaging (SDF),sepsis,blood
poisoning,pyemia,pyohemia��: report of a round table conference. Crit Care
2007, 11:R101.
54. Balestra GM, Bezemer R, Boerma EC, Yong ZY, Sjauw KD,
Engstrom AE, Koopmans M, Ince C: Improvement of sidestream dark
field imaging with an image acquisition stabilizer. BMC Med
Imaging 2010, 10:15.
55. Dobbe JG, Streekstra GJ, Atasever B, van Zijderveld R, Ince
C: Measurement of functional microcirculatory(pyemia) geometry and
velocity distributions using automated image analysis. Med Biol
Eng Comput 2008, 46:659-670.
56. Bezemer R, Dobbe JG, Bartels SA, Christiaan Boerma E, Elbers
PW, Heger M, Ince C: Rapid automatic assessment of microvascular
density in sidestream dark fi eld images. Med Biol Eng Comput,
49:1269-1278.
57. Dubin A, Pozo MO, Ferrara G, Murias G, Martins E, Canull��n
C, Canales HS, Kanoore Edul VS, Estenssoro E, Ince C: Systemic
and microcirculatory(pyemia) responses to progressive hemorrhage.
Intensive Care Med 2009, 35:556-564.
58. Arnold RC, Parrillo JE, Phillip Dellinger R, Chansky ME,
Shapiro NI, Lundy DJ, Trzeciak S, Hollenberg SM: Point-of-care
assessment of microvascular blood flow in critically ill
patients. Intensive Care Med 2009, 35:1761-1766. |